Company Biography
CP25 - Centralized Opioid Management and Behavioral Approaches to Treatment (COMBAT)
Poster Type: Innovation
Category: Public Health Crises
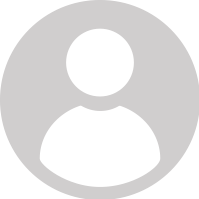
Issue or Challenge: Opioid use disorder (OUD) is a chronic disorder with potential consequences including disability, relapse, and death. Opioid overprescribing negatively impacts patients and increases the risk of physician licensure revocation. AltaMed, the largest federally qualified health center in Southern California, identifies over 150 patients for problematic opioid prescribing on a monthly basis. Consistent with CURES, criteria include multiple providers prescribing and over three months of opioid therapy. To ensure that evidence-based guidelines are followed consistently, the AltaMed Institute for Heath Equity launched the Centralized Opioid Management and Behavioral Approaches to Treatment (COMBAT) initiative in 2018 by braiding complementary grant funding streams.
Description of Innovation: Since 2018, the AltaMed Institute for Health Equity developed the infrastructure of complementary funding streams, capitalizing on funding from two Sierra Health Foundation grants, a CVS/NACHC grant, and four grants from the Health Resources and Services Administration. COMBAT is a multipronged approach addressing barriers to delivering and accessing OUD services in primary care settings. The initiative leverages funding to increase capacity for OUD services including Medicated Assisted Treatment (MAT), train a growing cohort of X-waivered physicians, fund pharmacy support, and reduce patient barriers to treatment, including financial support for transportation and medication. AltaMed has internally invested in personnel time and fostered support across clinics. These resources were used to pilot two models of care: MAT on Demand and Chronic Pain Clinics. The framework has facilitated the development of structural goals including the prevention of new opioid misuse cases through safe prescribing, avoidance of opioid deaths through harm reduction including Naloxone and Buprenorphine prescriptions, treatment of OUD with MAT, and implementation of a “no wrong door” care program for patients with chronic pain and other chronic conditions. Stakeholders are exposed to the larger COMBAT goals, decreasing organizational silos and increasing collaboration to standardize best treatment practices for both providers and patients.
Impact or Result: From December 2017 to March 2018, AltaMed had one Naloxone prescription. From December 2018 to March 2019 there were 132 Naloxone prescriptions and the number continues to rise. Since program inception, nine providers have received their X-Waiver. Each year, four providers are supported through X-Waiver training and mentored on MAT services implementation to increase capacity. Each provider can manage 30 MAT patients in their first year and apply for a larger patient load in following years. In 2019, capacity for MAT patients rose to 120 patients compared to no capacity prior to program implementation. This initiative has successfully leveraged collaboration across departments to dedicate hour-long physician schedule blocks for MAT walk-in patients. COMBAT has also resulted in the refinement of high-risk opioid use criteria; identification of physicians with high-risk prescribing patterns; development of opioid stewardship policies and procedures, workflows, scripts, referral pools and resources in EPIC; and building internal/external partnerships.
Replicating this Innovation: The AltaMed Institute for Health Equity envisions expanding COMBAT into a patient-centered, “no wrong door” OUD continuum of care that organizes treatment and support services at a pace that matches the patient’s level of readiness. This model will enable FQHCs to build departmental collaborations to expand OUD services and optimize the delivery MAT services in an integrated primary care setting to ensure that those who need it most can access it. The goal is to transition from grant funding to internal investment of the program. COMBAT is in early stages of development but provides important lessons learned for other organizations.
Author(s):
Marisol Frausto, MPH, Project Coordinator, AltaMed Health Services
Qiana Montazeri, MPH, Program Manager, AltaMed Health Services
Indira Sanchez, Grants Manager, AltaMed Health Services,
Aisli Valencia, Community Health Fellow, AltaMed Health Services
Rosa Argueta, Community Health Fellow, AltaMed Health Services
Contact Information
Team Members

Marisol Frausto
AltaMed Health Services
Project Coordinator
Qiana Montazeri
AltaMed Health Services
Program Manager
Indira Sanchez
AltaMed Health Services
Grants Manager

Aisli Valencia
AltaMed Health Services
Community Health Fellow